Posture follows movement like a shadow
Are you being double crossed by your posture? There is a chronic condition called Upper Crossed Syndrome (USC) which is expressed by the rounding of shoulders, forward chin poke of the head. Mostly seen with elderly, but with an accelerated escalation of sedentary lifestyles and work environments, it has become a common sight for all ages.
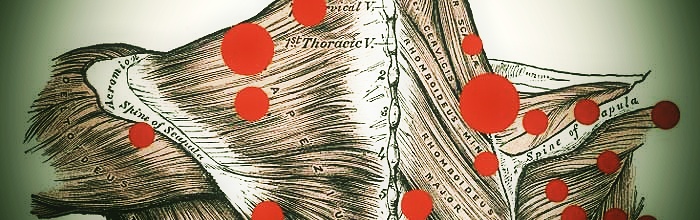
Upper Crossed Syndrome Anatomy
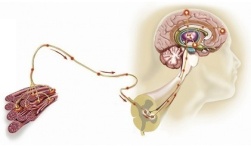
The position of your head and shoulder is orchestrated by various opposing forces. These muscle balance forces vary depending on the positions we regularly find ourselves in. With UCS there is usually a weakness of the deep neck flexors and overactive/tightness of the upper traps and levator scapulae. This causes a forward head position with a hinge point at the lower cervical spine.
Lower down with weakness of rhomboids and lower traps, matched with overactive/tight pectoralis major and minor causes a rounding of the shoulders.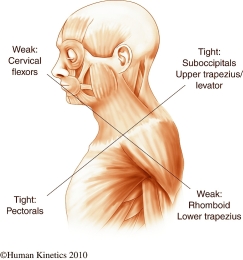
The muscle imbalance can affect multiple joint levels of the spine, the glenohumeral joint, the acromioclavicular joint and scapulothoracic joint. These might all lead to dysfunctions and result in injury.
How does this impact me?
Well that depends on how you live your life. This is a chronic condition that affects multiple joints and progressively over years they become stiff or weak. This closes the window on living an active lifestyle and increases risk of injury.
With less mobility and stability, comes greater risk to injury.
This is typical with most office workers, students or driver’s. Their neuromuscular system has adapted to the UCS shape for years. But the injury risk increases when activity and movement levels are pushed higher than normal, for example overhead lifting, throwing sports or freestyle swimming that requires a wider overhead range of movement and ends up putting undue stress on the upper body.
Have you got the following?
- Chin Poke: Is your head sticking so far out it’s at risk of falling off! Next time you stop at traffic lights take a look at the other drivers posture, it’s common to see the drivers head stuck at least 12 inches from the head rest.
- Rounding of the Shoulders: Due to a weakness of scapula retractors, the lower traps and rhomboids, the super tight Pec muscles draw the shoulders forwards. Look at overly developed bodybuilders for a great example of rounded shoulders.
- Winging scapula: When the scapula lifts away from the wall of the rib cage, it’s usually the result of a muscle imbalance. This might take a friend to spot this one for you.
- Creasing in the neck: It’s the last places you want to see a crease. At the base of the neck and accompanied by the start of a hump in the thoracic spine.
Change starts now – How do I get there?
Expecting to do an overhead squat or chest to bar pull up straight away might be unrealistic if you’ve spent years holding a UCS posture. But there are ways of getting there…
- Scaling the new movement that your practicing and working within the ranges that your body allows. Giving the joints time to adapt, without risking injury.
- Working on individual muscles that developed the weakness and tightness over the years. This requires specific strengthening and stretching exercises.
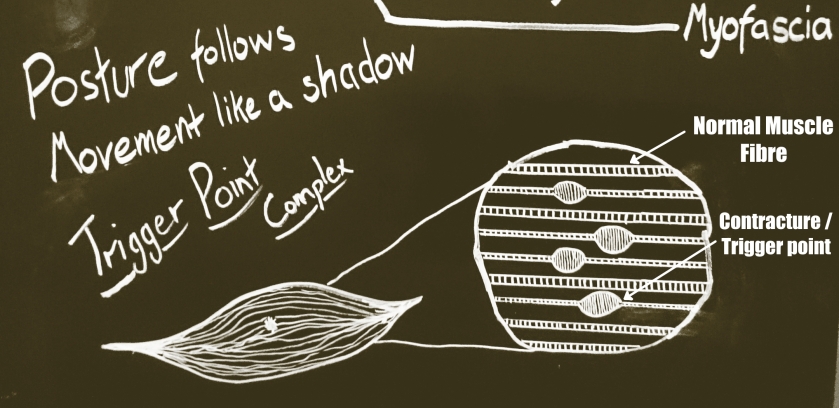
- Muscle tightness in your neck and chest may benefit from soft tissue work to release the muscle, like massage or dry needling.
- Correcting form, sometimes we don’t have the body awareness to identify poor technique. Having the coach or physio look at your movement to correct where it’s needed.
- Change can only be enforced through repetition and habit. The positions you’re in most of the day dictate your posture. At work, in the car, or at home, try to change your posture regularly.
Below are some basic examples of exercises to get you started with organising the shoulder and head. Try following them regularly to give your body the opportunity to change.
Continue reading “Upper Crossed Syndrome – A foundation for failure”

 Injury or pre-existing weakness can cause a guarding response from the nervous system.
Injury or pre-existing weakness can cause a guarding response from the nervous system.